Intermittent Fasting
Alternate Day Fasting


Modified Fasting Regimens
Time-Restricted Feeding
Ramadan Fasting
One of the five pillars of Islam is that healthy adult Muslims must fast from dawn to sunset during the holy month of Ramadan. In addition, fluid intake, cigarette smoking, and medications are forbidden.
Depending on the season and the geographical location of the country, day fasting can vary from 11 to 22 hours. Islamic fasting during Ramadan does not require energy restriction; however, as intake of food and fluid becomes less frequent, changes in body weight may ocures


Other Religious Fasts
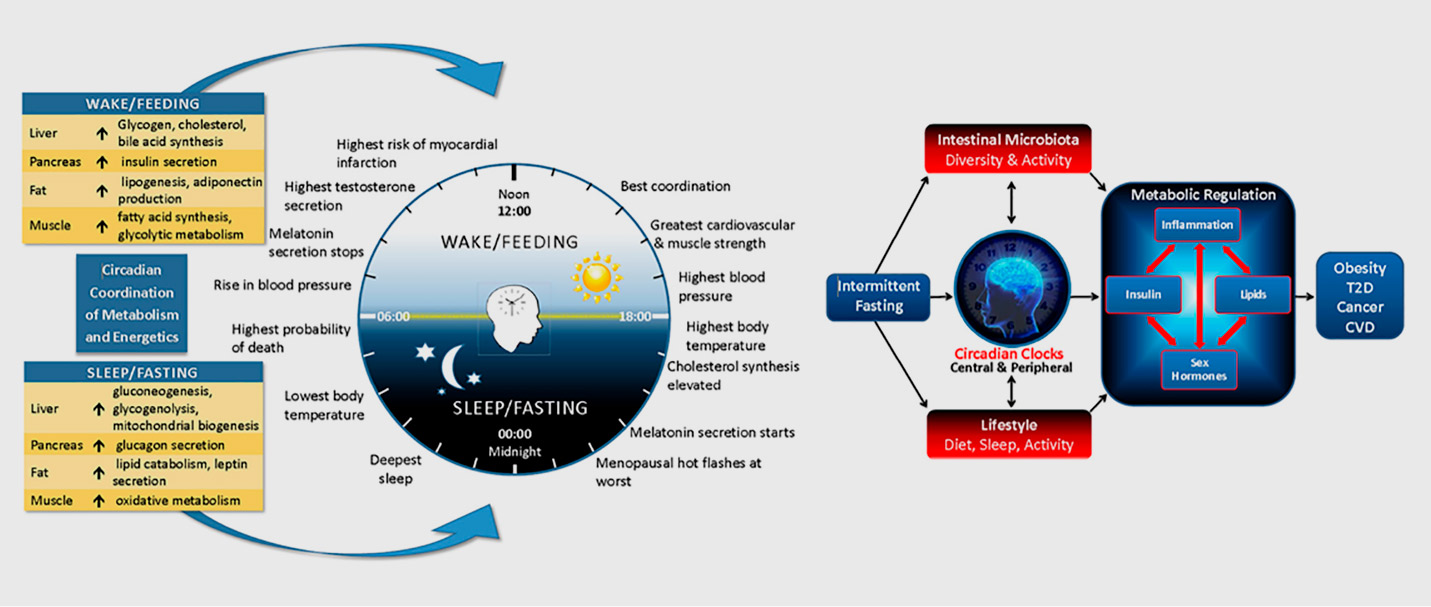
Circadian Biology
Gastrointestinal (Gut) Microbiota
Many functions of the gastrointestinal tract exhibit robust circadian or sleep-wake rhythms. For example, gastric emptying and blood flow are greater during the daytime than at night and metabolic responses to a glucose load are slower in the evening than in the morning. Therefore, it is plausible that a chronically disturbed circadian profile may affect gastrointestinal function and impair metabolism and health.
Intermittent fasting may directly influence the gut microbiota, which is the complex, diverse, and vast microbial community that resides in the intestinal tract. Studies suggest that changes in composition and metabolic function of the gut microbiota in obese individuals may enable an “obese microbiota” to harvest more energy from the diet than a “lean microbiota” and thereby influence net energy absorption, expenditure, and storage.


Modifiable Lifestyle Behaviors
ENERGY INTAKE
CONCLUSIONS
Copyright@ 2022 Gerald J. Joseph International, LLC - HealthCoach All Right Reserved

